Why do Industrial Hygienists think that Masks don't work as a Public Health response tool?
What are mitigation measures that actually work?
I feel like when dealing with the mainstream of people, friends, family, schools, it would be helpful to go back to basics to educate in a respectful way. Think of it as "undoing" the damage the propaganda media has done to the understanding of Covid mitigation measures. The media has mostly shown you Doctors' opinions on masks. They have not shown you Industrial Hygienist Occupational and Environmental Toxicology Expert statements. That's because this group has been entirely ignored during the Covid pandemic. One of these experts recently opened up her knowledge to a school board:

I've been "lucky" if you want to call it that because in the Spring of 2020 my first instinct was to look at the initial Covid particle size estimate and research what masks could handle in terms of mitigating tiny particles from entering the human respiratory system.
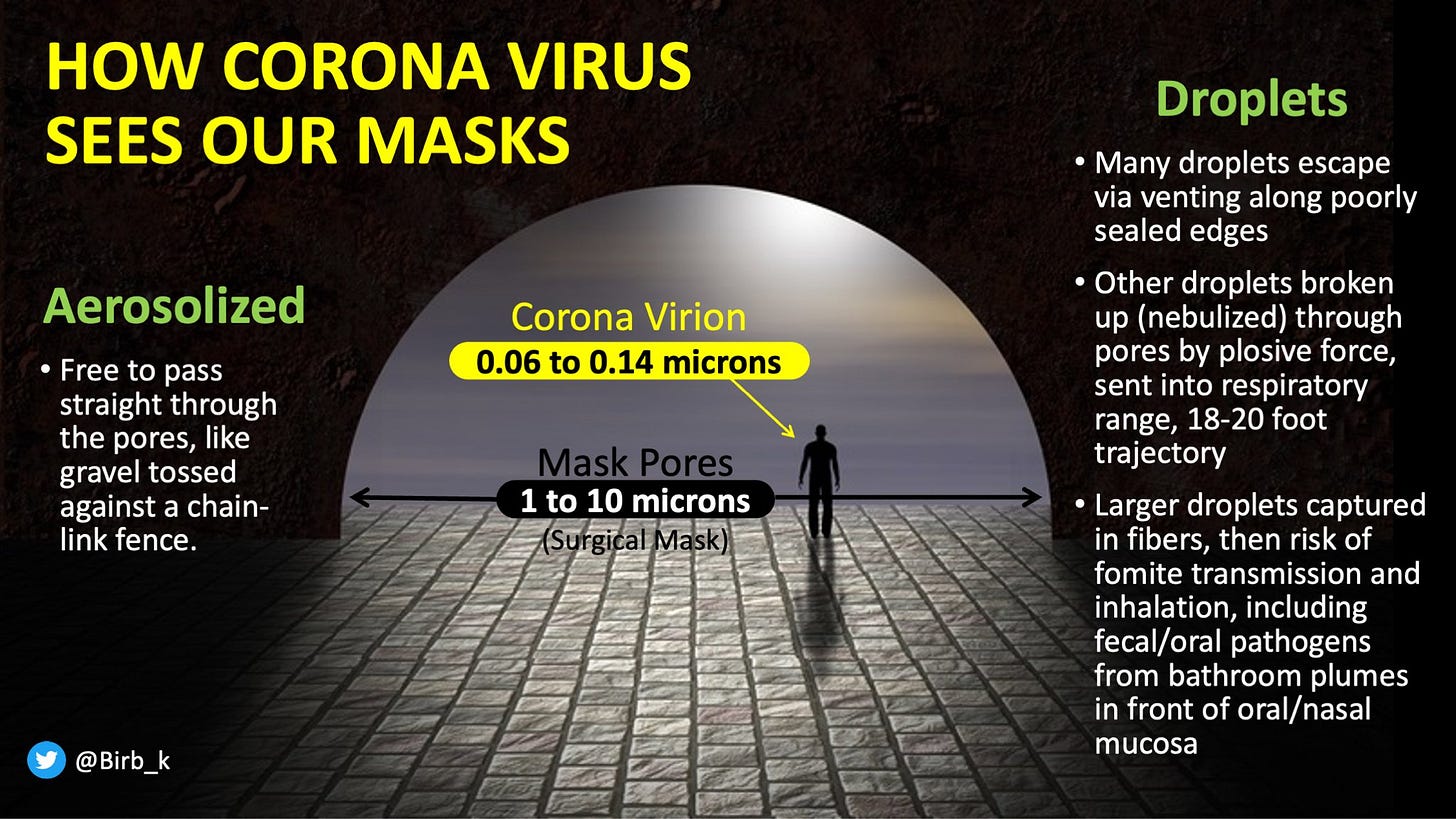
You've often seen it oversimplified by the "fence and mosquitos" meme, but the reality is more complex.
An indoor-air researcher at the University of Hong Kong, named Yuguo Li conducted research during the SARS outbreak, in 2003, his investigation revealing that an outbreak at the Amoy Gardens apartment complex provided the strongest evidence that a coronavirus could be airborne. He’d also struggled to convince the public health community that their risk calculus was off until he finally decided to work out the math. Li’s simulations showed that when a person coughed or sneezed, the heavy droplets were too few and the targets—an open mouth, nostrils, eyes—too small to account for many infections. Li’s team had concluded, therefore, that the public health establishment had it backward and that most colds, flu, and other respiratory illnesses must spread through aerosols instead.
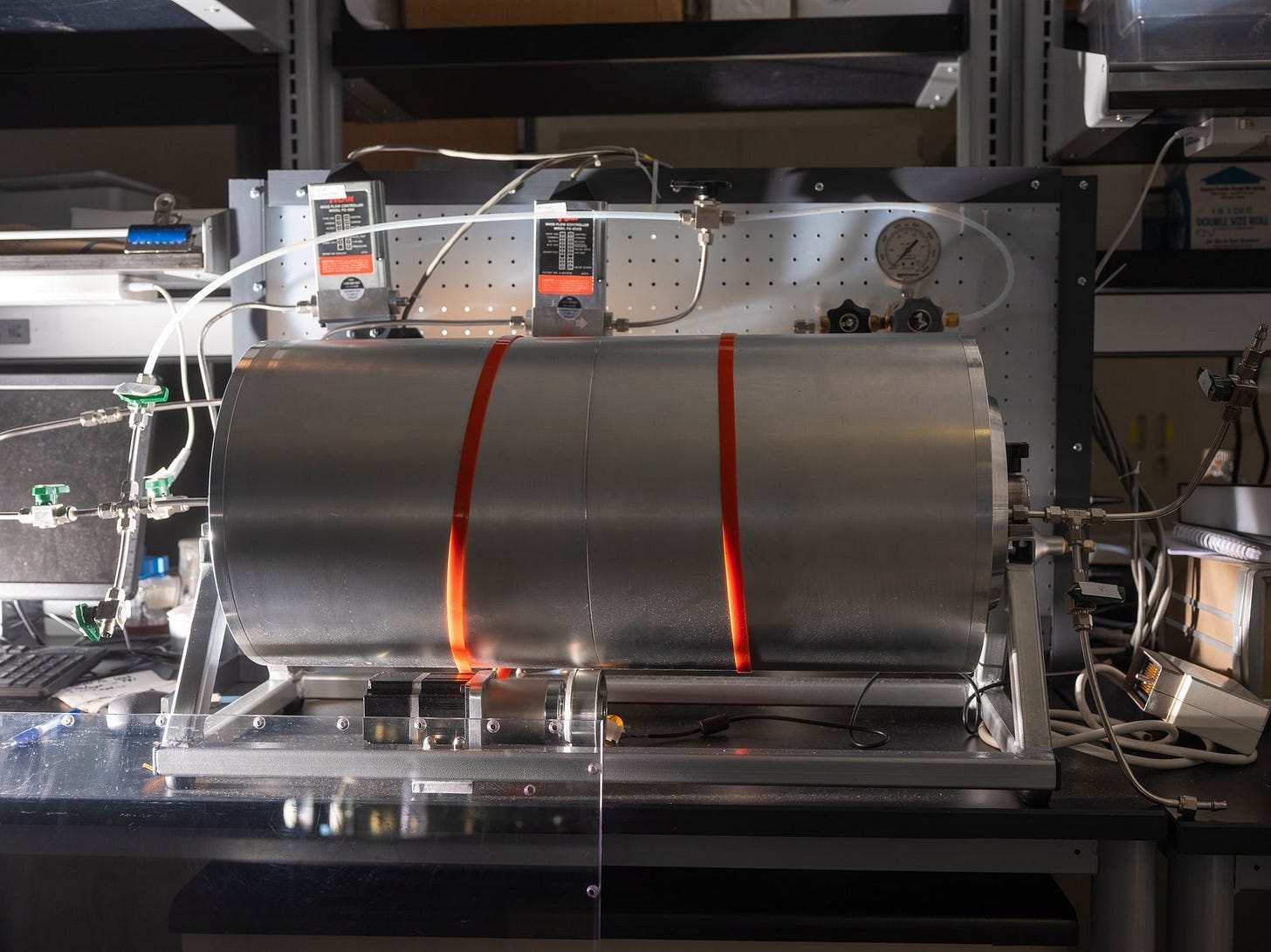
Pictured: A rotating drum to aerosolize viruses and study how well they survive under different conditions. PHOTOGRAPH: MATT EICH
When Scientists studying spread mechanisms of Sars-Cov-2 researched “5 microns” and “tuberculosis” in the CDC’s archives last year, they made a stunning historic discovery: a book written by a Harvard engineer named William Firth Wells. Published in 1955, it was called Airborne Contagion and Air Hygiene.
In 1934, Wells and his wife, Mildred Weeks Wells, a physician, analyzed air samples and plotted a curve showing how the opposing forces of gravity and evaporation acted on respiratory particles. They were able to predict the time it would take a particle of a given size to travel from someone’s mouth to the ground. Particles bigger than 100 microns sank within seconds. Smaller particles stayed in the air. The droplet-aerosol dichotomy should have pivoted around 100 microns, not 5.
Wells installed air-disinfecting ultraviolet lights inside schools. In the classrooms with UV lamps installed, fewer kids came down with measles. Conclusion: The Measles virus must have been in the air.
Alexander Langmuir, who joined the newly established CDC as an epidemiologist in 1949, was obsessed with Biological warfare, turning the focus of his research onto studies from the 1940s looking at the hazards of working in factories and mines, showing the mucus of the nose and throat to be exceptionally good at filtering out particles bigger than 5 microns. However, the smaller ones could slip deep into the lungs and cause irreversible damage. If someone wanted to turn a rare and nasty pathogen into a potential agent of mass infection, he wrote, they could easily formulate it into a liquid that could be aerosolized into particles smaller than 5 microns, tiny enough to bypass the body’s main defenses.
Well, too had written about those industrial hygiene studies: He investigated the role particle size played in the likelihood of natural respiratory infections, designing a study using tuberculosis-causing bacteria. The bug was hardy and could be aerosolized, and if it landed in the lungs, it grew into a small lesion. Exposing rabbits to similar doses of the bacteria, he pumped into their chambers either as a fine (smaller than 5 microns) or coarse (bigger than 5 microns) mist. The animals that got the fine treatment fell ill, and an autopsy revealed, it was clear their lungs bulged with lesions. The bunnies that received the coarse blast appeared no worse for the wear.
Scientists inside the CDC fused his observations by picking the size of the particle that transmits tuberculosis out of context, making 5 microns stand-in for a general definition of airborne spread. Wells’ 100-micron threshold got left behind.
In July of 2020 two women sent slides to Anthony Fauci. They showed the trajectory of a 5-micron particle released from the height of the average person’s mouth. It went farther than 6 feet—hundreds of feet farther. Just weeks later, speaking to an audience at Harvard Medical School, Fauci admitted that the 5-micron distinction was wrong—and had been for years, stating: “There is much more aerosol than we thought.” But the droplet dogma remained.
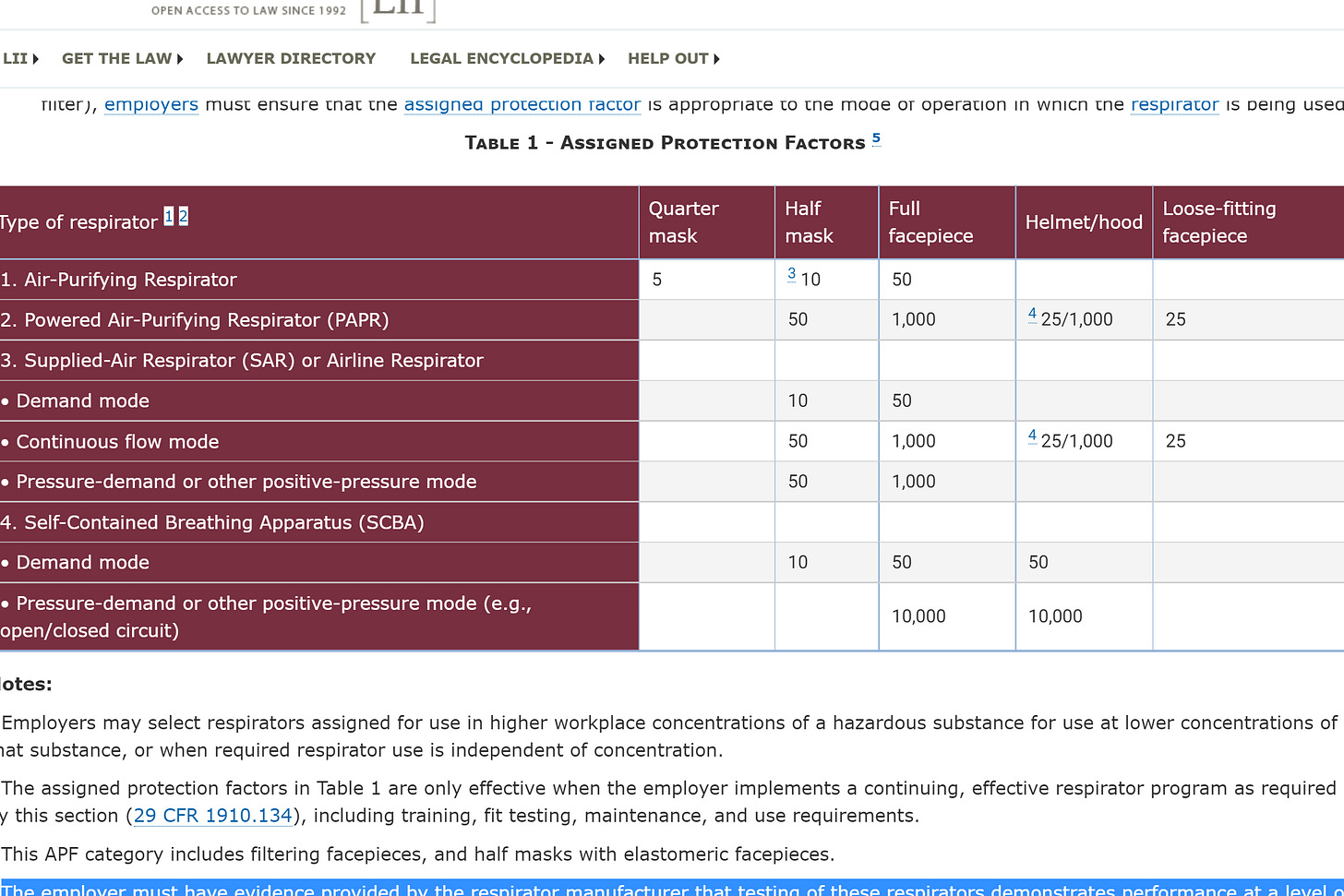
OSHA Standards demand that: Employers must use Assigned Protection Factors (APFs). to select a respirator that meets or exceeds the required level of employee protection. The employer must have evidence provided by the respirator manufacturer that testing of these respirators demonstrates performance at a level of protection of 1,000 or greater to receive an APF of 1,000. Industrial Hygienist access and license protection of such devices on a case by case basis, depending on the individuals’ personal health conditions.
After reading Wells's project with air-disinfecting ultraviolet lights inside schools, effectively killing Measles particles in the classrooms in the 1930s, I am left to wonder, with the magnanimous levels of Government spending on the Pandemic, how have we not figured out how to install a modern version of Well’s undertakings in every school?
The question begs, how after a full school year of open schools in some areas of the country, and the world, some of which in settings where students were not masked, how are we still having the same argument of masking?
The study “COVID-19 Mitigation Practices and COVID-19 Rates in Schools: Report on Data from Florida, New York, and Massachusetts”, emphasizes: “Ventilation improvements are correlated with lower COVID-19 rates in Florida”, and: “Further, we do not see a correlation between mask mandates and COVID-19 rates among students in either adjusted or unadjusted analyses.”
Germicidal UV-C Basics
For nearly a century, short-wave ultraviolet (UV) C (UV-C) energy—similar to sun rays—has been used to destroy airborne and surface-bound microbes, including chickenpox, measles, mumps, tuberculosis (TB), and cold viruses. Yet, despite decades of research and thousands of applications in hospital emergency and operating rooms, urgent-care centers, universities, and first-responder locations, UV-C has not been widely leveraged.
UV light is a band of electromagnetic radiation classified into four wavelength ranges: vacuum UV (100 to 200 nm), UV-C (200 to 280 nm), UV-B (280 to 315 nm), and UV-A (315 to 400 nm). Wavelengths from 100 nm to 280 nm are germicidal. At 253.7 nm (commonly referred to as “UV-C”), the UV wavelength changes the structure of DNA and RNA, the genetic code of all life forms, inhibiting the ability of cells to reproduce. While bacteria and viruses absorb UV-C energy at different rates, no microorganism tested to date has proven resistant when subjected to an appropriate dose.
Although UV-C energy has proven effective in inactivating other coronaviruses, such as the 2003 severe acute respiratory syndrome (SARS) and the 2012 Middle East respiratory syndrome (MERS), scientists have limited information about UV-C’s impact on SARS-CoV-2, the virus that causes COVID-19. Early indications from ongoing studies at Columbia University and elsewhere, however, indicate that “UV is very efficient for killing this virus.”
In May 2020, the Centers for Disease Control and Prevention (CDC) recommended to businesses preparing to reopen following the pandemic the use of germicidal UV to reduce the likelihood of disease transmission.
Source: https://www.amca.org/educate/articles-and-technical-papers/amca-inmotion-articles/uv-c-for-hvac-air-and-surface-disinfection-2.html
Where are the Media, Politicians, Foundations, advocating for the use of these systems, which could be argued to be the #1 Mitigation measure for the primary spread that occurs indoors, where ventilation is poor?
Where are the active advertising campaigns telling people that these systems are being Government funded in every school across the country reassuring parents on the safety of their children, as they are returning to classrooms this fall, instead of selling them the Illusion that masks in classrooms have any beneficial impact to the health and safety of kids?
Mission in action: A thorough enough education of the general, mask touching, population to understanding the Aerosolized spread, why cloth masking and 6 feet of distance don’t, and will never work for pathogens of that Virion size.